Campaign in Wales – An Introduction
In Wales, we appreciate the good work being undertaken by many good people within the NHS and understand the widespread issues are complex.
Like campaigners in other UK nations, we do not perceive the widespread NHS issues to be solely related to insufficient financial investment (indeed, as this recent study revealed more staff did not improve waiting times).
From our lived experiences, we believe key contributory factors to the concerning widespread issues to be cultural issues, inefficiencies and, moreover, a lack of independence and accountability when things go wrong.
Thus, our campaigners in Wales are calling for an Independent NHS Complaints Service (INCS) to be established in Wales, equipped with impartial staff with sufficient expertise and time to investigate patient and staff complaints and concerns in a truly open, honest, independent and timely manner, avoiding secondary harm to staff and patients, whilst ensuring optimal learning is identified, addressed and monitored consistently, in a meaningful way, and shared locally and nationally.
Health Services in Wales
Health is devolved in Wales and responsibility lies with the Senedd (Welsh Parliament) and Welsh Government. As Cabinet Health Secretary for Wales, Jeremy Miles, recently highlighted, “The day-to-day responsibility for running the health service, which includes treatment decisions about individuals, rests with health boards and NHS trusts.”
The following site provides an overview of the NHS structure in Wales, including: 7 Health Boards; 3 Trusts (including Welsh Ambulance Services including the 111 service); Special Health Authorities and other supporting bodies:
How is the NHS structured in Wales? | NHS Confederation
The Duty of Candour for NHS organisations in Wales was introduced in April 2023, almost a decade later than in England, and we wonder how Wales may differ in their understanding, monitoring and implementation of it.
Cabinet Health Secretary for Wales, Jeremy Miles, states “Adherence to this duty in Wales is monitored and challenged during oversight meetings by the Welsh Government and the NHS Executive to ensure that organisations can accurately report their performance against the duty.”
Many highlight concern around the duty of candour being distinct from the professional duty of candour, which places an obligation on healthcare professionals - as individuals - to be open and honest when things go wrong; individual professional duty of candour remains regulated by GMC/NMC/GDC etc. and was something highlighted in Findings of the call for evidence on the statutory duty of candour - GOV.UK The above report raises vital considerations for all UK nations, including:
- a professional duty of candour for NHS managers and on the existing statutory (organisational) duty of candour in respect of managers.
- a duty of candour on all public servants and officials, with criminal sanctions for the most serious breaches.
- wider recommendations to improve patient safety, including for the duty of candour to cover individuals in leadership positions in NHS organisations, and making them accountable for responding to concerns about patient safety.
Currently, concerns and complaints relating to health and social care in Wales are primarily dealt with via ‘Putting Things Right’ process Public Health Service Ombudsman Wales and Llais.
Wales currently do not have Martha’s Rule (based on Ryan’s Rule) but have ‘Call 4Concern’ initiative being rolled out.
Whilst our Welsh campaigners recognise some positive changes have been made over the years within Wales, they report experiencing issues that mirror those reported in the other 3 UK nations and join our call for an Independent NHS Complaints Service (INCS) to be established, to undertake patient and staff complaints and concerns in a truly open, honest and independent way.
Putting Things Right (PTR) process
Concerns about care or treatment in Wales are encouraged in the first instance to be resolved as soon as possible directly with the staff involved. Alternatively, patients complaints can be to the health board or trusts complaints team. The process for raising concerns or complaints in NHS Wales is called ‘Putting Things Right’, a procedure under which Public Health Wales manage and respond to ‘concerns’ with consideration of redress to meet the requirements of the NHS (Concerns, Complaints and Redress Arrangements) (Wales) Regulations 2011. The management of complaints or ‘concerns’ regarding NHS Wales care or treatment is governed by The National Health Service (Concerns, Complaints and Redress Arrangements) (Wales) Regulations 2011. The process for raising concerns or complaints in NHS Wales is called Putting Things Right.
The term “concern” is used throughout the PTR process and means “any complaint, claim or reported patient safety incident (about NHS treatment or services) to be handled under these arrangements. It also includes concerns which may also trigger the candour procedure as set out in the Duty of Candour Procedure Regulations 2023”.
The PTR process aims to address relatively minor complaints or concerns through to the most catastrophic (severe harm or death) under one process. The name ‘Putting Things Right’ has attracted much criticism and many complainants ask how can anything be ‘put right’ for a patient that experienced avoidable suffering and death due to NHS failures in care?
Following recent consultation, it appears the (rather unfortunate for some) name is here to stay, though work is in progress to redesign the PTR process, and the legislation and the guidance which governs it. The consultation responses included concerns around the quality of investigations undertaken and the quality of the training of those undertaking investigations, and have been confirmed as being part of the scope of the refresh and redesign work. Next steps to change the process in line with the feedback and ideas received is underway. It remains to be seen whether the changes will appropriately address current concerns, particularly those regarding the independence, training, and professional standards followed by investigators. As our campaigners believe to be the case across all UK nations, systems whereby NHS are largely expected to investigate their own failures, with insufficient accountability, are fundamentally flawed, with optimal learning often not being identified, monitored and maintained as a knock on effect, hence we see the same themes of repeated widespread failures.
Implementation and oversight of HR policies are outside the scope of Putting Things Right and remain the responsibility of CEOs. If a complainant is not satisfied with the health board or trust’s response, they can contact the Public Services Ombudsman for Wales.
Public Health Service Ombudsman Wales (PHSOW)
Cabinet Health Secretary for Wales, Jeremy Miles, recently highlighted, “The Public Services Ombudsman (Wales) Act 2019 has strengthened PSOW’s powers to independently investigate complaints. Where certain criteria are met, PSOW can undertake extensive investigations of a matter already under investigation, or a standalone investigation which does not relate to a complaint made by an individual.”
The link below, shares a 2023 report produced regarding poor complaints handling in Wales:
https://www.ombudsman.wales/blog/2023/06/15/today-we-publish-our-special-report-groundhog-day-2/
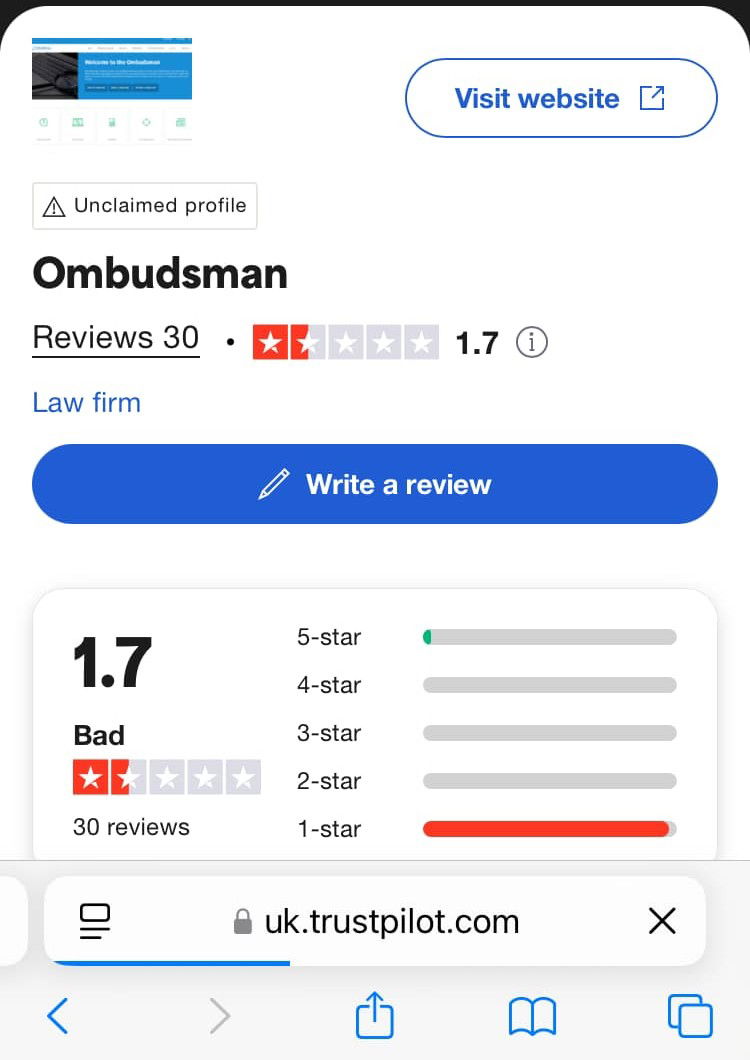
Our fellow campaign supporters in Wales have expressed concerns with PHSOW to England counterparts, including frustrations with reluctance to investigate and insufficient regulatory oversight or power to ensure implementation of their recommendations when they do investigate:
https://uk.trustpilot.com/review/www.ombudsman.wales
Ombudsman Reviews | Read Customer Service Reviews of www.ombudsman.wales
‘Llais’ – Free complaints advocacy and support in Wales
Llais (meaning 'Voice' in Welsh) is an independent body which provides free and confidential complaints advocacy and support, aiming to provide a positive contribution to strengthening voices of people going through the internal NHS complaints process and helping to shape services. There are, however, limitations as to what advocacy agencies such as Llais can do, including limited scope in providing advice and being unable to support anyone who has legal representation. Many experience these limitations as a gap, as the primary aim of legal representation (e.g. medical negligence Solicitors) is proving both breach of duty and causation for a successful case ‘win’ but often, what harmed patients and/or bereaved families want goes much deeper than this. In cases where admission of liability is formally accepted, harmed patients and bereaved families often report experiencing secondary harm and being left with unanswered questions and a lack of confidence that meaningful learning has been identified and appropriately addressed.
Whistleblowing
In 2023, Welsh Government published the Speaking Up Safely framework to strengthen and protect whistle-blowers within organisations in order to protect the person speaking out and form part of the culture of change and challenge for the NHS to achieve.
Some recent publicity related to whistleblowing in Wales:
Lucy Letby: New Welsh NHS whistleblowing guidance after case - BBC News
Brynmawr Medical Centre: Ex-practice manager speaks out | South Wales Argus
Death investigations
Death investigations : Coronial Process and Medical Examiner Service
A new statutory Medical Examiner Service has been rolled out across England and Wales to provide independent scrutiny of deaths, and to give bereaved people a voice. Whilst this is a positive introduction, some express concern that like scope is limited, along with the coronial process.
Coroners are required, by law, to investigate deaths which are suspected to have been violent or unnatural, where the cause of death is unknown, or where the person died while being detained by the state – for example, in prison, by the police, in immigration detention or in a mental health care facility. Coroners’ investigations are carried out to answer four questions: who died, how they died (including the medical cause of death), when they died, and where the death occurred. The final stage of some investigations is a fact-finding public hearing (an inquest.)
Jeremy Miles himself acknowledges limitations “A coroner’s inquest is a formal judicial inquiry into the case and circumstances of a death, and is a limited, fact-finding inquiry” and that “Coronial law and practice are the responsibility of the UK Government – that means only the UK Government can make changes to the system in Wales and England.”
Some of our Welsh campaigners have expressed concern with the limitations of the Coronial process within England and Wales. Providing an example of sepsis, dubbed ‘the biggest killer’, with over 48,000 individuals per year lose their lives to sepsis, often preventable with early detection and treatment, PHSO expressed recent concern that NHS are not learning from mistakes and a recent study of Coroner’s reports revealed 45% of Sepsis Prevention of Future Death Reports resulted in no response. Many others in Wales have raised concern that optimal learning is not happening across all nations. The following report touches upon this issue, and that of the inconsistencies with the service people receive depending on where they live:
Bereaved people are not yet at the heart of the coroner service
The duty of disclosure in coroners’ inquests is limited to the information requested by the coroner. These requests must be complied with under coronial law, but due to limited scope and potential for inconsistencies as highlighted above, if a coroner fails to request certain information deemed pertinent by the family, families can sometimes find themselves in the unfortunate situation of feeling the inquest has not provided them with full answers.
Our Stories: Wales
OUR WELSH SUPPORTERS
Silver Voices
Non-Profit Campaign Group for over 60s
We believe in self-representation by older people to advance our aims, rather than relying on the charities to speak for us Silver Voices is the only independent, individual membership organisation for senior citizens in the UK. MPs, councillors and many other opinion-formers receive our briefings and our influence is growing all the time. We are unashamedly political but not affiliated to any political party. Politicians from all parties have let older people down and age discrimination is still rife at all levels of society. There is a special responsibility on those of us whose parents fought for and built the Welfare State to help prevent it being dismantled in front of our eyes. We will campaign for an improved public NHS and a solution to the social care crisis as our first priorities.
Families Failed by OUH Maternity Services
Campaigners & Advocates
Families Failed by OUH Maternity Services is a campaign advocating for a full independent inquiry into the systemic failures within Oxford University Hospitals Maternity Services
Speak Up Now UK
Campaign Group supporting Whistleblowers
https://www.speakupnowuk.com/ Our MISSION is to provide a platform where people can share their stories so that we can provide transparency on what is actually going on in our public services and also to enable a sense of relief and support to anyone going through discrimination etc at their workplace and feel that it has not been properly dealt with correctly.
Dr Max Mclean
Former Chair of Bradford Teaching Hospitals NHS Trust; Former Police Detective
Whistle-blower and campaigner for patient safety, focusing on Maternity care. Removed from his position of Chair, following the raising of safety concerns, all proven by an independent investigation.
Will Powell
Campaigner for Robbie's Law
I am campaigning for Robbie's Law, which would make it a legal requirement for ALL Healthcare Profess to be truthful following a medical error.
SPOTLIGHT JUSTICE
Supporting victims of NHS & Social Care Abuses
Supporting victims of NHS & Social Care Abuses and Police and Judicial Corruption. #WhateverItTakes #TheyMatterToUs #ActionNotSympathy
Sue Alison
NHS WB, seeking the truth
Sue become a Public Governor at University Hospitals of Morecambe Bay in 2021. Driven by a desire to improve safety for both patients and staff after her own career was destroyed as a consequence of whistleblowing about patient harm
Dr Chris Day
Locum Emergency Medicine Doctor
Husband, Dad, Doctor, Crowdfunder. "Fight for the things that you care about, but do it in a way that will lead others to join you" @54kdoctor
Dear Coroner
Former NHS Governor pioneers 'Dear Coroner' Upholding Nolan Principles, unveiling concealed truths in a deeply entrenched, toxic culture
Illuminate shadows, safeguard lives, champion the public interest. Join us, and bring a lamp? A beacon shining light into darkness. #UnveilingTruth #DearCoroner